DISCLAIMER: Mito Red Light devices are Class II wellness devices aimed at affecting the body through topical heating and supporting cellular function. The information provided in this article and on this site is for educational purposes only and is not intended to imply effectiveness of Mito Red Light devices for any specific application. The information provided in this article and on this site is not intended to diagnose, treat, cure, or prevent any disease, is not a substitute for consultation with a licensed medical provider and should not be construed as medical advice. Click here to read our article on potential contraindications of red light therapy..
Authored By Benjamin Caleb Williams
Muscle recovery is a vital consideration for anyone who is serious about fitness or athleticism. One important tool that is becoming popular to improve the speed and effectiveness of muscle recovery is red light therapy. This new form of therapy is being used by many people, from professional athletes whose careers depend on their physical condition to ordinary people wanting to get the most out of their workouts.
Red light therapy has been an emerging beneficial health modality since the mid-1990s. Red light therapy has its origins in NASA research [1], when researchers using red light to promote plant growth found that it also helped researchers’ wounds to heal faster after prolonged exposure to red light. While red light therapy is now used for a variety of health reasons, including sleep quality, pain control, and better skin quality, its original use of speeding healing remains the most relevant for improving athletic performance.
Musculoskeletal System Overview
Muscle recovery centers around the musculoskeletal system. This system of the body includes not only muscles but also bones, ligaments, tendons, cartilage, and connective tissues. Muscles do not function by themselves, and each component of the musculoskeletal system interacts with other components, ultimately affecting muscle health.
The entire musculoskeletal system [2] serves as a frame for the body, allowing for movement and the manipulation of one’s environment. The musculoskeletal system includes:
- Bones - The skeleton provides the frame for the entire body, giving solid structure to each extremity, our heads and faces, and our core. Bones are essential for movement and serve as the solid, stable frame that all our soft biological tissues depend on to remain in place within our body.
- Muscles - While the skeleton is important for providing structure, muscles are what actually moves that structure. All muscles except the tongue are long structures that have two ends, both of which connect to bones. Muscle cells can forcefully contract, allowing bones to change their position in relationship to each other.
- Joints - Joints are where two bones contact each other and can move against each other. There are many different kinds of joints. Joints can be very simple, like the hinge joint in the elbow that only moves back and forth. They can also be relatively complex, like the ball and socket hip and shoulder joints that allow for a wide range of motion in any direction.
- Tendons - Tendons are connective tissues that join muscles to bones. Muscle tissue does not directly bind to bone tissue, and tendons connect these two different tissue types. Tendons do not contract like muscles and serve a purely connective role.
- Ligaments - Ligaments are very similar to tendons, but instead of connecting muscles to bones, they connect bones to other bones. Ligaments are responsible for many important functions, such as keeping the two bones in your forearms parallel and aligned with each other and in place. Ligaments serve to keep bones stationary relative to each other, while tendons and muscles allow bones to move relative to each other.
- Cartilage - Cartilage is a slippery, elastic tissue that covers the end of each bone where there is a joint. Cartilage is vital for ensuring that bones glide smoothly over each other without causing friction. Without cartilage, bones in joints would grate against each other, causing friction and pain that would make smooth motions difficult or even impossible.
Muscles
As the primary drivers of motion, muscles [3] play the most important role in our ability to move and control the environment around us. Muscles generally consist of linear-appearing cells that are arranged in the same orientation. When activated by the nervous system, muscle cells change shape, going from long and thin to short and thick. This change in the cells can be seen on a larger scale by the effect it has on a muscle’s size and shape when it is flexed versus when it is extended.
Muscle cells can only contract and cannot extend by themselves. This makes it necessary for muscles to operate in pairs, with one that can contract in one direction and one that can contract in the opposite direction. With the exception of the tongue, all skeletal muscles will always connect to at least two bones that are able to move in relationship to each other. Because muscles do not act independently, most exercises are focused on groups of muscles rather than individual muscles.
Skeletal muscles are the main type of muscle that is important to consider relating to muscle recovery and exercise. This type of muscle is the only type of muscle under conscious control. There are other types of muscle that are under unconscious control and do not generally join two joints together. Muscles like the heart, the stomach, and the lining of the arteries and veins are all examples of non-skeletal muscles.
Muscles and Exercise
Exercising [4] improves the performance of your muscles in different ways. Most exercise focuses either on endurance, the ability to maintain a muscle contraction or to repeat it many times, or on strength, the ability of a muscle to move with more force. Many common forms of exercise, such as pushups, running, and swimming, are all endurance exercises. Strength exercises generally focus on lifting increasingly large weights.
During exercise, muscle performance is generally improved by the body increasing circulation to the muscles or by the muscles becoming damaged at a microscopic level and repairing themselves with greater muscle mass. The increasing mass of a muscle due to increased use is called hypertrophy, while decreasing muscle mass is called atrophy.
Muscle Recovery
Muscle damage occurs every time an exercise pushes a muscle beyond what it is accustomed to. Microscopic muscle damage is a normal and desirable outcome of exercise that will ultimately lead to improved function in the future. These tears, however, make the muscle weaker and sorer until the muscles heal. Exercising before the muscle has healed can lead to further damage that does not allow the muscle to recover or improve its function. This can inhibit the effectiveness of exercise and can even increase the risk of injury occurring.
Muscle recovery is often an important consideration for high-performance athletes who want to see improvements as fast as possible and who want to get the most out of their workouts. Optimizing muscle recovery allows for more frequent workouts, which improves muscle function more quickly.
Muscle recovery can also be a vital consideration when an injury occurs. Unlike microscopic tears in the muscle that heal within hours to days, a larger injury can take several days or even weeks to heal. This can seriously impede a workout program and create a significant setback. Rapid healing is important in these situations to minimize disruptions to workout programs.
Muscle-Related Injuries
Muscle-related injuries [5] can seriously affect a workout program, and understanding how to recover from these types of injuries is vital for athletes at any level. Muscle-related injuries are not injuries to the muscles exclusively and include injuries to the connective tissues that the muscles require to function and the joints that the muscles move.
Strains
A muscle strain [6] is a form of muscle-related injury that occurs to either the muscle or a tendon attaching the muscle to bone. A strain is sometimes informally referred to as a pulled muscle. Strains occur when the stress placed on a muscle is more than the muscle can handle, causing tearing in the muscle or tendons due to overstretching.
Strains can generally be distinguished from typical post-workout pain because the pain that develops from a strain occurs immediately after the injury instead of several hours to a day afterward, as would be expected from post-workout pain. Strains are graded according to their severity:
- Grade 1 (mild strain) - The muscles have been overstretched, and tears develop in the fibers. These tears are small but go beyond the microscopic tears that normally occur during workouts.
- Grade 2 (moderate strain) - Tearing is more serious; however, there is no complete tear in the muscle. Pain, swelling, and bruising are likely, limiting mobility.
- Grade 3 (severe strain) - Severe strains occur when most of the muscle fibers are torn or when there is a complete tear in the muscle or tendon. This serious form of injury can severely limit motion and may require surgery to repair.
Treating a strain depends on the severity of the strain. For most minor strains, treatment involves elevating the affected extremity, resting it, applying ice for up to twenty minutes at a time, and compressing it to decrease swelling. Over-the-counter pain medication can be used to control discomfort. Strains that do not quickly heal or seem serious should be evaluated and treated by a doctor.
Avoiding strains is always better than having to treat a strain. Avoiding overworking a muscle group, placing excessive strain on a muscle, or working out too frequently can all help to reduce the risk of strains. Contact sports increase the risk of strains, and precautions should be taken to avoid injury in these situations.
Sprains
Sprains [7] are sometimes confused with strains but are a different type of injury. While strains affect muscles and tendons, sprains affect the ligaments that bind bones together. Sprains often occur because the stress on the ligaments is too much, causing them to overstretch. Muscles play a role in most sprains, as the ligaments depend on muscles to help maintain the stability of the joint and reduce strain on the ligaments.
Sprains often manifest as a joint suddenly giving out and moving beyond its normal limits. Most sprains affect the ankles, especially when the ankle and leg are not aligned when the weight of the body comes down on the foot. This can be referred to as “rolling” your ankle, a motion that places stress on the ligaments and can lead to a sprain.
Sprains can occur in various levels of severity and are graded based on how severe they are:
- First-degree sprain (mild strain) - Minimal damage to the ligaments has occurred. Healing will typically be quick, and the sprain can often be treated by yourself.
- Second-degree sprain (moderate strain) - At least one ligament has been damaged, but no ligaments are completely torn. Partial tears are likely to be present. Healing will take longer, and bruising and swelling are likely to be noticeable.
- Third-degree sprain (severe strain) - At least one ligament has been completely torn. It may be impossible to fully use the damaged joint, and treatment may include a cast, brace, or even surgery.
The way a sprain is treated will depend entirely on how severe the sprain is. The RICE mnemonic (Rest, Ice, Compress, Elevate) can be used for most mild sprains to enhance healing and reduce pain. Over-the-counter pain medications may be used for pain control. More serious sprains may require prolonged rest periods, braces, casts, or even surgery.
Sprains can be avoided by taking several different measures. One of the best ways to avoid sprains is to maintain consistent muscle strength. Strong muscles help to maintain the structure and position of your joints, keeping everything in place. Avoid exercising when your muscles are weak or when you are tired, as your muscles will not be able to provide the same degree of stability. Having good footwear and braces to stabilize joints that are at risk can also reduce the risk of sprains.
Cramps
Cramps [8] are sudden, involuntary contractions of a muscle or group of muscles. Cramps are called exercise-induced cramps when they occur during exercise. Cramps can be painful but rarely cause any kind of lasting damage. They do, however, inhibit normal movements and can make it difficult or impossible to continue an activity. This can be very undesirable for athletes who are in the process of competing.
The cause of cramps is not fully understood, and there are several different ideas about what actually causes cramps to develop. There are, however, two main medical theories as to what causes exercise-induced muscle cramps:
- Fatigue - The most recent theory of the cause of cramps is that muscle fatigue causes changes in how nerves control muscle contractions. This leads the nerve signals to cause prolonged contraction that is not under conscious control.
- Electrolyte imbalance - Chemicals in the body called electrolytes are essential to healthy muscle activity. As we sweat during strenuous exercise, we lose fluids and electrolytes. Dehydration also causes electrolyte concentration changes. It is theorized that changes in electrolytes due to sweating and dehydration are the cause of exercise-induced muscle cramps.
A muscle cramp will normally resolve within minutes of stopping the use of the muscle, but there are some interventions that may cause them to resolve more quickly. Gently stretching the cramping muscle can help the muscle to relax and cause the cramp to dissipate. Drinking water can also help cramping resolve.
Avoiding cramps is important, especially when you are competing or when they are likely to affect your workout routine. There are some precautions that you can take to reduce the chances of getting cramps. These include:
- Staying well hydrated with water that contains replacement electrolytes
- Stretching well prior to exercising and warming up
- Avoid hot, strenuous conditions
Cramps are ultimately unlikely to be serious; however, frequent cramping may indicate that the exercises that you are doing are too strenuous or that you have an electrolyte imbalance that should be addressed.
Tendinitis
Tendonitis [9] is inflammation of the tendons and generally develops with the repetition of a specific movement over prolonged periods of time. Tendinitis goes by many nicknames, including tennis elbow, golfer’s elbow, pitcher’s shoulder, and swimmer’s shoulder. Most of the sports that tendinitis is associated with involve repetitive movements of a particular joint.
Medical scientists do not know exactly what causes tendinitis. Overuse of a joint, injury, or strain may all contribute to its development. When tendinitis does occur, inflammation of the tendon develops, causing it to become irritated and sore. If tendonitis is not treated and continues to worsen, your tendon could eventually rupture, causing the muscle to become partially or fully detached from the bone. This complication of tendinitis often requires surgery to repair.
Tendinitis may resolve on its own without any medical treatments; however, it could require medical intervention. Ice, rest, elevation, compression, and over-the-counter pain medications may be sufficient to help symptoms resolve in mild cases. Some of the potential treatments for tendinitis include:
- Adjusting activities to avoid repetitive use of the tendon
- Using a splint or brace to reduce movement of the tendon
- Applying ice for up to 20 minutes at a time to reduce inflammation and pain
- Steroid injections at the tendon to reduce inflammation and pain
- Physical therapy to help optimize muscle and tendon function
- Ultrasonic treatments that break up tendon scar tissue to facilitate healing
- Surgery to repair a torn or damaged tendon
Everyone’s situation will be different, and because of the seriousness of the potential problems that tendinitis can cause, anyone who has tendinitis should see a doctor to ensure they are getting correctly treated.
The risk of tendinitis can be reduced using several different strategies:
- Improve your technique - Tendinitis is often the result of repetitive activities. Poor technique can increase irritation caused by repetitive activities and increase the risk of tendinitis.
- Reduce intensity - If tendinitis may be starting to develop, reducing the use of the affected tendon can help to prevent more serious tendinitis from occurring.
- Change your exercise routine - Repetition is a key cause of tendinitis. Changing your exercise routine to avoid repetitive motions can reduce your tendinitis risk.
- Stretch - Stretching before an exercise can reduce the irritation that your exercise creates on your tendons, reducing your risk of tendinitis.
- Strengthen - Strengthening your muscles can help to reduce the stress on individual tendons, reducing the overall risk of tendinitis developing.
Optimizing Muscle Recovery
Anyone doing any kind of regular workout should carefully consider how to optimize muscle recovery. This is especially vital for serious athletes who must optimize every facet of their routine but is also important for anyone wanting to get the most out of their physical exercise.
There are many factors that influence the overall health and function of your muscles. These factors will affect the likelihood that muscle damage will occur while exercising and will influence how rapidly the muscles will recover after workouts and after injuries.
Hydration
Hydration is an important part of muscle function and helps to promote good muscle health. Research indicates [10] that staying hydrated not only improves athletic performance and endurance but also helps to promote muscle recovery after a workout.
Sleep
Getting enough high-quality sleep each night promotes muscle health and recovery. Research shows [11] that sleep can affect protein synthesis, a vital component of muscle recovery. Sleep also is known to promote healing and increases the speed of recovery from many different kinds of injuries and illnesses.
Massage
Massage has been shown to speed muscle recovery [12] after workouts. Massage helps to increase blood flow to muscles and increases the speed at which lactic acid that builds up in the muscles can be absorbed. This leads to decreased muscle soreness after working out and may increase the speed of muscle recovery.
Rest
Rest periods are important between workouts to allow microscopic muscle damage time to heal. Having adequate recovery time between workouts promotes muscle recovery [13] and improves the effectiveness of workouts.
Nutrition
Nutrition is a vital part [14] of any serious workout regimen. Building muscle and healing muscle requires protein to build the physical structure and energy to sustain healing. There are several important nutritional considerations for muscle recovery:
- Protein - Protein is the building block that provides muscle cells with their structure. Without protein, muscle cells and structure cannot correctly develop. Having an adequate intake of protein, especially immediately after a workout, is necessary to optimize the body’s ability to build new muscle.
- Carbohydrates - Carbohydrates provide the fuel and energy necessary for muscles to function and recover. Optional energy intake will reduce the amount of recovery needed by promoting muscle health during a workout and will also improve the ability to heal after a workout.
- Avoid processed sugars - Processed sugars, like corn syrup or high fructose corn syrup, are associated with increased inflammation. Sodas and sweets are high in processed sugars and can cause inflammation and decreased recovery following workouts.
- Balance - Ultimately, a nutritious diet centers around balance, requiring a balanced intake of healthy fats and oils, fruits, vegetables, proteins, and supplements. Professional athletes often focus heavily on maintaining a balanced diet that promotes muscle function while avoiding potentially inflammatory foods.
Avoid Drugs & Alcohol
Recreational drugs, alcohol, and tobacco can interfere with muscle recovery [15] in many different ways. The actual effect depends on the specific substance; however, most recreational substances cause stress on the body and affect its ability to heal and maintain optimal function.
Red Light Therapy
Red light therapy is becoming increasingly recognized as an effective method of speeding muscle recovery in athletes. Professional organizations, like the San Francisco 49ers, are beginning to install red light therapy panels in their locker rooms as the competitive advantage that the increased speed of muscle recovery it provides becomes more widely recognized.
Red Light Therapy and Muscle Recovery
There is a wide body of research supporting the use of red light therapy to not only promote muscle recovery but also to reduce muscle damage and improve performance during exercise. A 2016 article [16] published in the Journal of Biophotonics even raised the question if red light therapy should be permitted in athletic competitions without being regulated due to the potentially unfair advantage it could provide.
The key areas of research where red light therapy has been examined the most are its ability to reduce muscle damage, its ability to reduce muscle fatigue during and after exercise, its ability to improve performance during exercise, and its ability to improve muscle recovery. Each of these areas is inextricably interrelated and offers its own distinct benefits to muscle recovery.
How Red Light Therapy Works
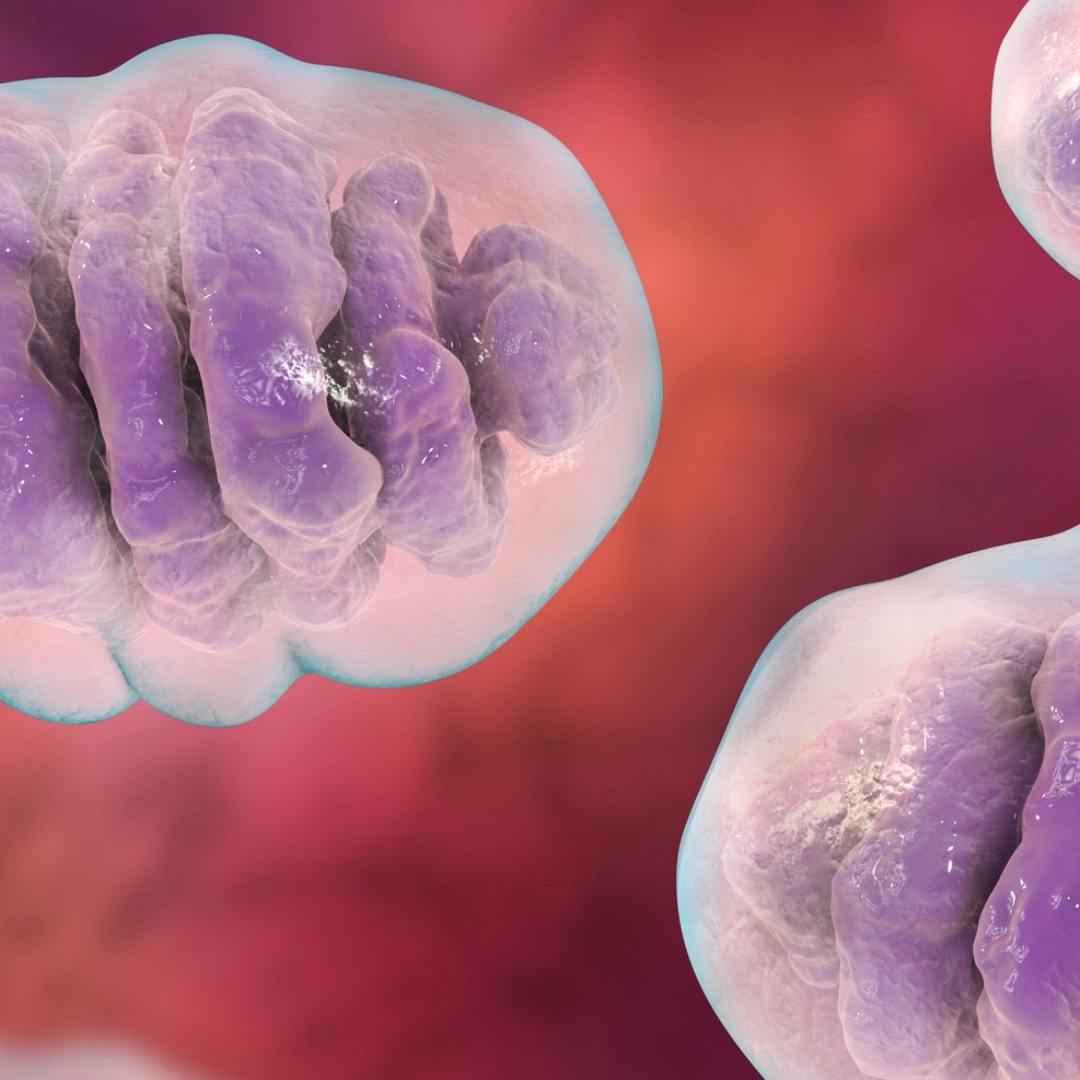
Red light therapy is thought to work by stimulating mitochondria [17], tiny organs found in each cell of the body. These subcellular organs are responsible for energy production, and a key chemical found in mitochondria called cytochrome C oxidase has been shown to absorb light within red and infrared wavelengths.
While research into how red light therapy works is still ongoing, the effects it has on mitochondria are thought to be what speeds healing and reduces pain. While this effect was first discovered in healing skin wounds, red light penetrates deep into muscle tissues, providing this benefit to muscles as well.
Reduced Muscle Damage
Many studies indicate that using red light therapy can potentially reduce muscle damage that can occur during exercise. This can lead to increased endurance and make workouts more productive. A 2010 article [18] in the European Journal of Applied Physiology found that using red light therapy prior to eccentric exercises led to a reduced level of biomarkers associated with muscle damage when compared to those who did not use red light therapy.
Other studies have yielded similar results. A study [19] published in Lasers in Medical Science used a double-blind, randomized, placebo-controlled experiment that found infrared light decreased inflammatory markers after exercise by water polo athletes. A 2019 experiment [20] also published in Lasers in Medical Science and using a randomized, crossover, double-blinded, placebo-controlled trial found that using red light therapy prior to a soccer match decreased the likelihood of developing hamstring injuries.
There are several other important studies that demonstrate the benefits that red light therapy can provide in reducing muscle damage. These studies also show that red light therapy can improve the speed at which muscles heal after being damaged or facilitate healing with certain muscle-related diseases. Some of these studies include:
- A 2020 review [21] published in the Journal of Sport Rehabilitation. This review explored research on the effects of red light therapy when used on soccer athletes. The researchers found specific doses of between 10 and 50 Joules of energy used after play provided the greatest effect. The review noted the need for further study to determine if there was a difference between how males and females respond to red light therapy.
- A review [22] published in MOJ Orthopedics & Rheumatology in 2015. This review found that the use of red light therapy to manage musculoskeletal pain had a strong basis of scientific evidence supporting its use. The review noted the limitations of red light therapy when there were actual structural deficits and further noted that red light therapy may be less effective with certain types of neurological causes of muscle.
- A 2013 study [23] in Laser Therapy. This study examined the effectiveness of red light therapy in treating sports injuries in a hospital setting. The study involved 41 patients and showed a 65.9% effectiveness rate for all sports injuries. The study also showed an even higher rate of effectiveness of the Jumper's knee, tennis elbow, and Achilles tendinitis and demonstrated that red light therapy was particularly promising for these conditions
- A 2021 narrative review [24] published in Research, Society and Development. This review analyzed evidence for the muscle-related effects of red light therapy. Important findings about the effects of red light therapy included that it treated muscle atrophy, potentially stimulating the growth of muscle cells, enhancing the formation of muscle fibers, and improving the process of eliminating old or damaged cells.
- A 2014 study [25] published in PLOS One. This study researched the effects of red light therapy on mice. The mice were treated with red light therapy five times a week for 14 months. Researchers found that this treatment resulted in “decreased morphological changes, skeletal muscle damage and inflammation” in the treated mice when compared to the control group. The researchers noted that their findings indicated that red light therapy held the potential to “decrease progression of Duchenne muscular dystrophy,” a muscle condition that is difficult to treat effectively.
Improved Muscle Performance
While research is quite clear that red light therapy seems to offer a protective effect against muscle damage during exercise, it also strongly indicates that it actually improves muscle performance during activity. This would extend the potential length of a workout while improving joint stability and safety during exercise.
Research [26] published in Lasers in Medical Science in 2009 showed that using red light therapy prior to exercise reduced the onset of muscle fatigue. A 2014 study [27] published in Photomedicine and Laser Surgery showed that the use of infrared light during rest intervals while exercising increased resistance to muscle fatigue. In 2019, research [28] in the International Journal of Sports Physiology and Performance showed that red light therapy increased the time it took for competitive cyclists to begin feeling exhausted.
Other important studies on the effects of red light therapy on muscle performance include:
- A twin case study [29] published in the American Journal of Physical Medicine and Rehabilitation. Using identical twins, this study showed that the use of red light therapy “increased the maximal load in exercise and reduced fatigue.” The research also demonstrated that there were decreased markers of inflammation and muscle atrophy in the twin that used red light therapy.
- A 2012 review [30] published in Photonics & Lasers in Medicine. This study examined a wide body of scientific literature and found that red light therapy can “improve muscle performance, reduce muscle fatigue during exercises, and benefit muscle repair.” The review also found that people with diseases like Duchenne muscular dystrophy may benefit from using red light therapy.
- A 2020 study [31] published in the Annals of Applied Sport Science. This study followed 50 individuals and used a double-blinded, controlled study methodology to show that using red light therapy resulted in a statistically significant decrease in blood lactate levels, muscle pain severity, and the perceived exertion of fatigue during and after exercise. The researchers concluded that using red light therapy before exercise “may improve muscular performance and reduce muscle soreness and fatigue.”
- A study published in 2023 in Nature. This double-blinded, controlled study followed 47 participants who had osteoarthritis, a painful joint condition that benefits from exercise. The researchers found that using red light therapy improved muscle strength and functional performance when compared to the control group. The researchers ultimately suggested that red light therapy be “integrated into rehabilitation programs to improve muscle strength and functional performance” for those with knee osteoarthritis.
Muscle Recovery After Exercise
While red light therapy has been demonstrated to reduce damage and improve performance during exercise, leading to improved athletic performance, it has also been demonstrated to have positive effects after working out. These positive effects primarily center around improved post-workout muscle recovery.
A 2014 study [33] published in Lasers in Medical Science used a randomized, double-blinded, placebo-controlled trial to demonstrate that a single treatment of red light therapy improved muscle soreness, muscle strength loss, and range of motion impairments caused by exercise. The effects were found to last for up to 96 hours after exercise.
Another study [34], published in 2016 in The Journal of Strength and Conditioning Research, used a randomized, crossover, double-blind, placebo-controlled clinical study examining the effects of red light therapy on rugby players. The study found that red light therapy meaningfully accelerated the muscle recovery of rugby players who had used red light therapy.
Other important studies into using red light therapy to improve postworkout recovery include:
- A 2010 study [35] published in the Journal of Orthopaedic & Sports Physical Therapy. This study followed 9 volleyball players who received pre-exercise red light therapy treatment. Researchers concluded that this treatment resulted in increased endurance and improved postexercise levels of important muscle-related blood markers.
- 2013 research [36] published in the Journal of Rehabilitation Research and Development. This study used lab rats to examine the effects of red light therapy. Researchers demonstrated that using red light therapy “positively affects injured skeletal muscle in rats, accelerating the muscle-regeneration process.”
- A review [37] published in Sports Health in 2022. This meta-analysis reviewed 24 randomized, controlled trials. The review found that using red light therapy before exercise resulted in decreased soreness after exercise. The review also identified at least three exercise-related biomarkers that were improved by the use of red light therapy.
- A 2018 study [38] published in Lasers in Medical Science. This study used a rat model to examine the effects of red light on muscle tissues. Rats that had been treated with red light therapy for seven days were found to have better distribution and organization of collagen, a connective protein essential for optimal muscle function. The researchers concluded that red light therapy had a positive effect on the muscle repair process.
- A 2013 review [39] published in the Journal of Athletic Training. This review analyzed data from controlled studies on red light therapy, ultimately finding that the use of red light therapy provided protective and post-exercise recovery benefits.
A study [40] published in the International Journal of Sports Physical Therapy in 2022. This controlled study followed 33 participants. The effects of red light therapy prior to sprinting were evaluated, and the researchers found that using red light therapy relieved muscle soreness in some muscle groups following exercise. The researchers also found that red light therapy was not as effective for reducing muscle soreness associated with “explosive, short-duration activities.”
Mito Red Light
Not all red light therapy panels are created equal. For red light therapy to be worth the investment, you need a high-quality, independently tested, professional red light therapy device from a reputable company. With over 5 years in business and over 65,000 ecstatic customers, Mito Red Light is a brand you can trust. Our reviews speak for themselves and you can also click to review some of our customers' red light therapy before and after examples.
We are confident that our devices are the highest quality and best value you’ll be able to find anywhere. We welcome you to review our selection of red light therapy devices or to contact one of our representatives at 1-866-861-6486 to learn more or to help find the right solution for you.
Related Articles:
- How Does Red Light Therapy Affect the Body?
- Red Light Therapy - Sleep, Energy and Performance
- An Overview of Uses of Red Light Therapy
References:
-
- NASA. (2022, May 19). NASA Research Illuminates Medical Uses of Light. Retrieved from https://spinoff.nasa.gov/NASA-Research-Illuminates-Medical-Uses-of-Light
- Villa-Forte, A. (n.d.). Introduction to the Biology of the Musculoskeletal System - Bone, Joint, and Muscle Disorders. Merck Manuals Consumer Version. Retrieved from https://www.merckmanuals.com/home/bone,-joint,-and-muscle-disorders/biology-of-the-musculoskeletal-system/introduction-to-the-biology-of-the-musculoskeletal-system
- SEER Training Modules. (n.d.). Introduction to the Muscular System. Retrieved from https://training.seer.cancer.gov/anatomy/muscular/
- Johnston, B. (n.d.). Overview of Exercise - Fundamentals. Merck Manuals Consumer Version. Retrieved from https://www.merckmanuals.com/home/fundamentals/exercise-and-fitness/overview-of-exercise
- Fernandes, T. L., Pedrinelli, A., & Hernandez, A. J. (2011). Muscle injury – Physiopathology, diagnosis, treatment and clinical presentation. Revista Brasileira de Ortopedia, 46(3), 247-255. https://doi.org/10.1016/S2255-4971(15)30190-7
- Noonan, T. J., & Garrett, W. E. Jr. (1999). Muscle Strain Injury: Diagnosis and Treatment. Journal of the American Academy of Orthopaedic Surgeons, 7(4), 262-269. https://journals.lww.com/jaaos/Abstract/1999/07000/Muscle_Strain_Injury__Diagnosis_and_Treatment.6.aspx
- Vuurberg, G., Hoorntje, A., Wink, L. M., van der Doelen, B. F. W., van den Bekerom, M. P., Dekker, R., et al. (2018). Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British Journal of Sports Medicine, 52(15), 956. https://bjsm.bmj.com/content/52/15/956
- Maughan, R. J., & Shirreffs, S. M. (2019). Muscle Cramping During Exercise: Causes, Solutions, and Questions Remaining. Sports Medicine (Auckland, N.Z.), 49(Suppl 2), 115–124. https://doi.org/10.1007/s40279-019-01162-1
- Almekinders, L. C. (1998). Tendinitis and Other Chronic Tendinopathies. Journal of the American Academy of Orthopaedic Surgeons. https://journals.lww.com/jaaos/Abstract/1998/05000/Tendinitis_and_Other_Chronic_Tendinopathies.3.aspx
- udge, L. W., Bellar, D. M., Popp, J. K., Craig, B. W., Schoeff, M. A., Hoover, D. L., Fox, B., Kistler, B. M., & Al-Nawaiseh, A. M. (2021). Hydration to Maximize Performance and Recovery: Knowledge, Attitudes, and Behaviors Among Collegiate Track and Field Throwers. Journal of Human Kinetics, 79, 111–122. https://doi.org/10.2478/hukin-2021-0065
- Dattilo, M., Antunes, H. K. M., Medeiros, A., Mônico Neto, M., Souza, H. S., Tufik, S., & de Mello, M. T. (2011). Sleep and muscle recovery: Endocrinological and molecular basis for a new and promising hypothesis. Medical Hypotheses, 77(2), 220-222. https://doi.org/10.1016/j.mehy.2011.04.017
- Naderi, A., Aminian-Far, A., Gholami, F., Mousavi, S. H., Saghari, M., & Howatson, G. (2020). Massage enhances recovery following exercise-induced muscle damage in older adults. Scandinavian Journal of Medicine & Science in Sports, 31(3), 623-632. https://doi.org/10.1111/sms.13883
- American College of Sports Medicine. (n.d.). A Road Map to Effective Muscle Recovery. American College of Sports Medicine. https://www.acsm.org/docs/default-source/files-for-resource-library/a-road-map-to-effective-muscle-recovery.pdf
- Jäger, R., Kerksick, C. M., Campbell, B. I., Cribb, P. J., Wells, S. D., Skwiat, T. M., Purpura, M., et al. (2017). International Society of Sports Nutrition Position Stand: protein and exercise. Journal of the International Society of Sports Nutrition, 14(20). https://jissn.biomedcentral.com/articles/10.1186/s12970-017-0177-8
- Lakićević, N. (2019). The Effects of Alcohol Consumption on Recovery Following Resistance Exercise: A Systematic Review. Journal of Functional Morphology and Kinesiology, 4(3), 41. https://doi.org/10.3390/jfmk4030041
- Ferraresi, C., Huang, Y.-Y., & Hamblin, M. R. (2016). Photobiomodulation in human muscle tissue: an advantage in sports performance? Review Journal of Biophotonics, 9(11-12), 1273-1299. https://doi.org/10.1002/jbio.201600176
- Tafur, J., & Mills, P. J. (2008). Low-Intensity Light Therapy: Exploring the Role of Redox Mechanisms. Photomedicine and Laser Surgery, 26(4), 323–328. https://doi.org/10.1089/pho.2007.2184
- Baroni, B. M., Leal Junior, E. C. P., De Marchi, T., Lopes, A. L., Salvador, M., & Vaz, M. A. (2010). Low level laser therapy before eccentric exercise reduces muscle damage markers in humans. European Journal of Applied Physiology, 110(4), 789-796. https://doi.org/10.1007/s00421-010-1562-z
- Zagatto, A. M., Ramos, S. de P., Nakamura, F. Y., de Lira, F. S., Lopes-Martins, R. Á. B., & Carvalho, R. L. de P. (2016). Effects of low-level laser therapy on performance, inflammatory markers, and muscle damage in young water polo athletes: A double-blind, randomized, placebo-controlled study. Lasers in Medical Science, 31(3), 511-521. https://doi.org/10.1007/s10103-016-1875-1
- Dornelles, M. P., Fritsch, C. G., Sonda, F. C., Johnson, D. S., Leal-Junior, E. C. P., Vaz, M. A., & Baroni, B. M. (2019). Photobiomodulation therapy as a tool to prevent hamstring strain injuries by reducing soccer-induced fatigue on hamstring muscles. Lasers in Medical Science, 34(6), 1177-1184. https://doi.org/10.1007/s10103-018-02709-w
- Bettleyon, J., & Kaminski, T. W. (2020). Does Low-Level Laser Therapy Decrease Muscle-Damaging Mediators After Performance in Soccer Athletes Versus Sham Laser Treatment? A Critically Appraised Topic. Journal of Sport Rehabilitation, 29(8), 1210–1213. https://doi.org/10.1123/jsr.2019-0421
- Cotler, H. B., Chow, R. T., Hamblin, M. R., & Carroll, J. (2015). The Use of Low Level Laser Therapy (LLLT) For Musculoskeletal Pain. MOJ Orthopedics & Rheumatology, 2(5), 00068. https://doi.org/10.15406/mojor.2015.02.00068
- Morimoto, Y., Saito, A., & Tokuhashi, Y. (2013). Low level laser therapy for sports injuries. Laser Therapy, 22(1), 17-20. https://doi.org/10.5978/islsm.13-OR-01
- Gonçalves, S. R., Tim, C. R., Martignago, C. C. S., Silva, M. C. P., Anaruma, C. A., & Garcia, L. A. (2021). Potential of photobiomodulation therapy in the treatment of skeletal muscle atrophy. Research, Society, and Development, 10(1). https://doi.org/10.33448/rsd-v10i1.8527
- Leal-Junior, E. C. P., de Almeida, P., Tomazoni, S. S., de Carvalho, P. T. C., Lopes-Martins, R. Á. B., Frigo, L., Joensen, et al. (2014). Superpulsed Low-Level Laser Therapy Protects Skeletal Muscle of mdx Mice against Damage, Inflammation and Morphological Changes Delaying Dystrophy Progression. PLOS One. https://doi.org/10.1371/journal.pone.0089453
- Leal Junior, E. C. P., Lopes-Martins, R. A. B., Vanin, A. A., Baroni, B. M., Grosselli, D., De Marchi, T., Iversen, V. V., & Bjordal, J. M. (2009). Effect of 830 nm low-level laser therapy in exercise-induced skeletal muscle fatigue in humans. Lasers in Medical Science, 24(3), 425-431. https://doi.org/10.1007/s10103-008-0592-9
- Vieira, W. H. de B., Bezerra, R. M., Queiroz, R. A. S., Maciel, N. F. B., Parizotto, N. A., & Ferraresi, C. (2014). Use of low-level laser therapy (808 nm) to muscle fatigue resistance: A randomized double-blind crossover trial. Photomedicine and Laser Surgery, 32(12), 678-85. https://doi.org/10.1089/pho.2014.3812
- Lanferdini, F. J., Bini, R. R., Baroni, B. M., Klein, K. D., Carpes, F. P., & Vaz, M. A. (2018). Improvement of Performance and Reduction of Fatigue With Low-Level Laser Therapy in Competitive Cyclists. International Journal of Sports Physiology and Performance, 13(1), 14-22. https://doi.org/10.1123/ijspp.2016-0187
- Ferraresi, C., Bertucci, D., Schiavinato, J., Reiff, R., Araújo, A., Panepucci, R., ... & Bagnato, V. (2016). Effects of Light-Emitting Diode Therapy on Muscle Hypertrophy, Gene Expression, Performance, Damage, and Delayed-Onset Muscle Soreness: Case-control Study with a Pair of Identical Twins. American Journal of Physical Medicine & Rehabilitation, 95(10), 746-757. https://doi.org/10.1097/PHM.0000000000000490
- Ferraresi, C., Hamblin, M. R., & Parizotto, N. A. (2012). Low-level laser (light) therapy (LLLT) on muscle tissue: performance, fatigue and repair benefited by the power of light. Photonics Lasers in Medicine, 1(4), 267-286. https://doi.org/10.1515/plm-2012-0032
- Abedi Yekta, A. H., Tabeii, F., Salehi, S., Sohrabi, M.-R., Poursaeidesfahani, M., Hassabi, M., ... Mahdaviani, B. (2021). Effect of Low-Level Laser Therapy on Muscle Strength and Endurance and Post-Exercise Recovery of Young Adult: A Double-Blind, Placebo-Controlled, Randomized Clinical Trial. Annals of Applied Sport Science, 9(2), e912. https://aassjournal.com/article-1-912-en.pdf
- Jankaew, A., You, Y.-L., Yang, T.-H., Chang, Y.-W., & Lin, C.-F. (2023). The effects of low-level laser therapy on muscle strength and functional outcomes in individuals with knee osteoarthritis: A double-blinded randomized controlled trial. Scientific Reports, 13(165). https://doi.org/10.1038/s41598-022-26553-9
- Borges, L. S., Cerqueira, M. S., Rocha, J. A. dos S., Conrado, L. A. L., Machado, M., Pereira, R., ... & Neto, O. P. (2014). Light-emitting diode phototherapy improves muscle recovery after a damaging exercise. Lasers in Medical Science, 29(3), 1139-1144. https://doi.org/10.1007/s10103-013-1486-z
- Pinto, H. D., Vanin, A. A., Miranda, E. F., Tomazoni, S. S., Johnson, D. S., Albuquerque-Pontes, G. M., ... & Leal-Junior, E. C. (2016). Photobiomodulation Therapy Improves Performance and Accelerates Recovery of High-Level Rugby Players in Field Test: A Randomized, Crossover, Double-Blind, Placebo-Controlled Clinical Study. Journal of Strength and Conditioning Research, 30(12), 3329-3338. https://doi.org/10.1519/JSC.0000000000001439
- Leal Junior, E. C. P., Lopes-Martins, R. Á. B., Frigo, L., De Marchi, T., Rossi, R. P., de Godoi, V., ... & Bjordal, J. M. (2010). Effects of Low-Level Laser Therapy (LLLT) in the Development of Exercise-Induced Skeletal Muscle Fatigue and Changes in Biochemical Markers Related to Postexercise Recovery. Journal of Orthopaedic & Sports Physical Therapy, 40(8), 524-532. https://www.jospt.org/doi/10.2519/jospt.2010.3294
- Rodrigues, N. C., Assis, L., Fernandes, K. R., Magri, A., Ribeiro, D. A., Brunelli, R., ... & Renno, A. C. M. (2013). Effects of 660 nm low-level laser therapy on muscle healing process after cryolesion. Journal of Rehabilitation Research and Development, 50(7), 985–996. https://www.rehab.research.va.gov/jour/2013/507/pdf/jrrd-2012-08-0147.pdf
- Luo, W.-T., Lee, C.-J., Tam, K.-W., & Huang, T.-W. (2022). Effects of Low-Level Laser Therapy on Muscular Performance and Soreness Recovery in Athletes: A Meta-analysis of Randomized Controlled Trials. Sports Health, 14(5), 687–693. https://doi.org/10.1177/19417381211039766
- de Brito, A., Alves, A. N., Ribeiro, B. G., Barbosa, D. V. D. E., Magalhaes, E. M. R., Fernandes, K. P. S., ... & Mesquita-Ferrari, R. A. (2018). Effect of photobiomodulation on connective tissue remodeling and regeneration of skeletal muscle in elderly rats. Lasers in Medical Science, 33(3), 513-521. https://doi.org/10.1007/s10103-017-2392-6
- Borsa, P. A., Larkin, K. A., & True, J. M. (2013). Does phototherapy enhance skeletal muscle contractile function and postexercise recovery? A systematic review. Journal of Athletic Training, 48(1), 57–67. https://doi.org/10.4085/1062-6050-48.1.12
- D’Amico, A., Silva, K., Rubero, A., Dion, S., Gillis, J., & Gallo, J. (2022). The Influence of Phototherapy on Recovery From Exercise-Induced Muscle Damage. International Journal of Sports Physical Therapy, 17(4), 658–668. https://doi.org/10.26603/001c.34422