DISCLAIMER: Mito Red Light devices are not clinically proven to diagnose, treat, cure, or prevent any medical conditions. Mito Red Light devices are low / risk general wellness devices aimed at affecting the body through supporting cellular function. The scientific studies referenced in this article are for educational and informational purposes only and are meant to educate the reader on the exciting and growing field of phototherapy. To see a list of precautionary warnings and contraindications, click here
Table of Contents
- What is Inflammation?
- Inflammatory Response
- Symptoms of Inflammation
- Cause of Inflammation
- Chronic Inflammation
- Inflammatory Diseases
- Red Light Therapy and Inflammation
- How Might Red Light Therapy Help Inflammation?
- How is Red Light Therapy Used?
- Mito Red Light
- References
People commonly use red light therapy as a means of reducing inflammation and the pain that it causes. Red light therapy is a newer form of therapy that was only recently discovered by NASA researchers [1] in the 1990s when experimentation on using red light to enhance plant growth was also found to improve wound healing by the scientists running the experiments.
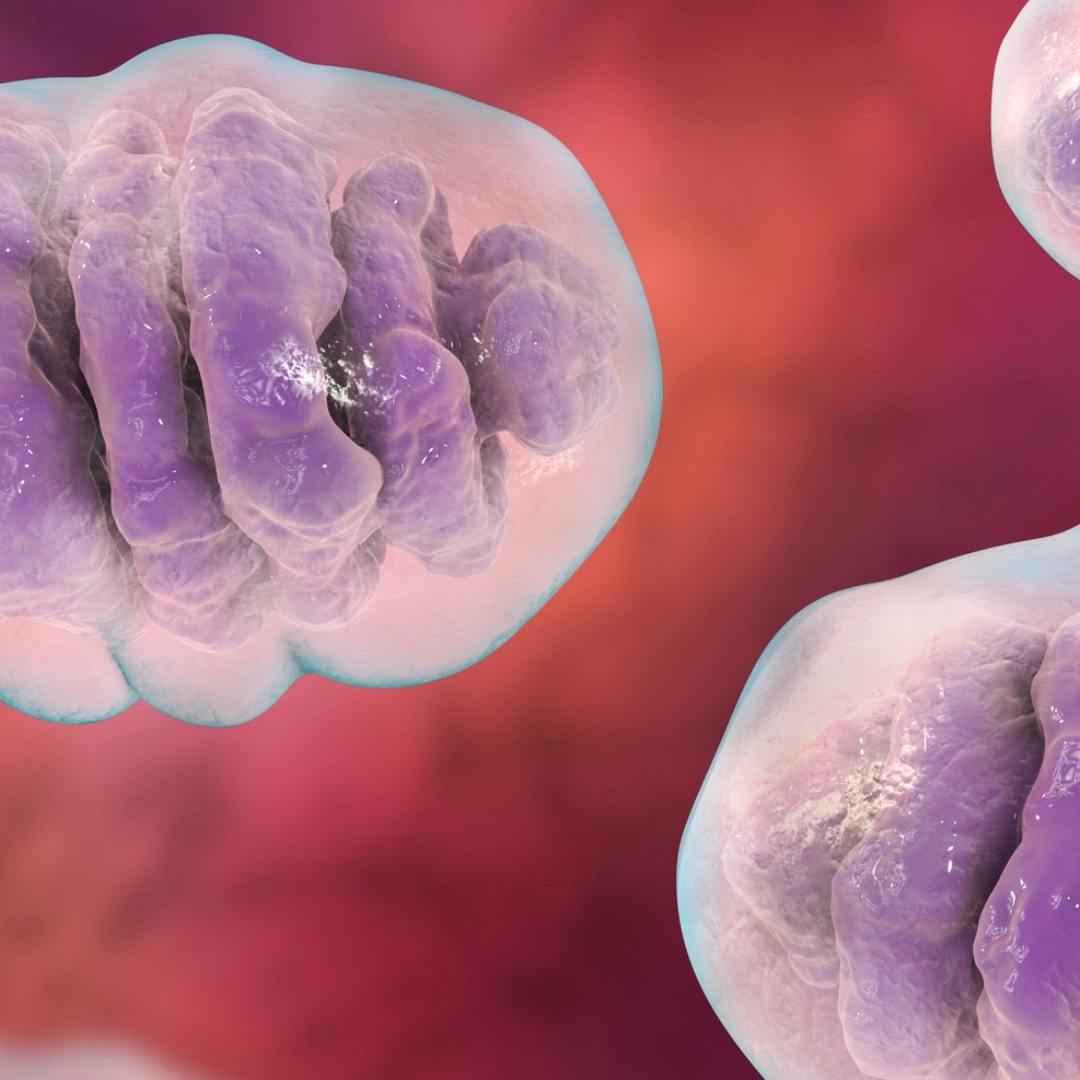
Red light therapy essentially involves using red and infrared wavelengths of light that are irradiated on the area being treated. The specific wavelengths of light used in red light therapy are thought to stimulate mitochondria [2]. These small, subcellular organs play an important role in producing energy in every cell and helping to suppress inflammation.
What is Inflammation?
While inflammation is a commonly-used medical term, many people do not fully understand what inflammation is and what causes it. Inflammation is part of the immune response and plays a vital role in helping the body respond to injury. Inflammation is actually a healthy and necessary part of how the body heals itself, but it can also become a chronic problem when the body consistently stays in an inflamed state.
Inflammatory Response
Your body’s first line of defense is your skin. The skin keeps out bacteria and other harmful organisms, separating the contents of your body from the outside world. When the skin is injured, the inflammatory response [3] occurs to repair the skin barrier and to minimize damage caused by the injury.
The inflammatory response first occurs when damaged cells release chemicals to signal that damage has occurred. These chemicals include histamine, bradykinin, and prostaglandins. These chemicals help to signal the immune cells that damage has occurred, drawing them to the area to deal with bacteria and other pathogens that can enter into the damaged area.
In addition to signaling the immune system to respond, chemical mediators increase blood flow to the area by making blood vessels dilate, causing increased nutrients and chemicals necessary for blood clotting to be available for initial healing.
Another important component of the immune response is that the chemicals involved in signaling cause the blood vessels around the damaged area to become more leaky, causing swelling in the tissues around the injury. This helps to isolate any foreign substances in the area, increases the delivery of chemicals and immune cells to the area, and creates a pain signal that helps you realize that there is an injury that needs to be attended to.
While inflammation often occurs as the result of an external injury, it can also be internal, caused by a chemical irritation or damage that the body responds to. Bacteria and viruses can also activate the inflammatory response, helping the immune system respond quickly and effectively.
Symptoms of Inflammation
Inflammation [4] can cause several important symptoms. These include:
- Swelling - The tissues in the inflamed area will generally become swollen and squishy. This effect is caused by blood vessels becoming more leaky.
- Warmth - The inflamed area will generally be warm to the touch and warmer than the surrounding skin. This effect is caused by increased blood flow during inflammation.
- Drainage - During initial inflammation, a clear drainage may occur at the site of the injury. This is due to the increased swelling and fluid in the area of the injury. Later in the process, pus may develop as immune cells kill bacteria.
- Pain - Pain is a common problem with inflammation but serves an important purpose, telling your body that a problem is present. Pain generally occurs because swelling creates pressure in the tissues.
Cause of Inflammation
Inflammation can have several different causes. The extent to which inflammation occurs is dependent on what triggers it and how well the body is able to respond to the trigger. Potential causes of inflammation include:
- Injury - Injuries that cause mechanical damage to any part of the body will trigger inflammation. This will typically involve a break in the skin but can also involve organs that are damaged by the injury.
- Chemicals - Exposure to certain chemicals can activate the inflammatory response. While the chemical is generally described as causing the inflammation, it is typically injuries created by the chemical that actually cause the inflammation.
- Burns - Burns are a unique kind of injury that causes inflammation. Severe burns lead to serious fluid loss, as the swelling caused by inflammation is not retained in the tissues, but leaks out continuously.
- Infection - Infection can cause inflammation, even if there is not an injury. The immune system’s response to an infection leads to inflammation in the area affected. Severe infections in the bloodstream can trigger a serious type of inflammation called systemic inflammatory response syndrome that causes inflammation throughout the body and can be fatal.
- Autoimmune - Autoimmune diseases activate the body’s immune response against part of your own body. This leads to a similar type of inflammation as infection but damages your body instead of invading bacteria.
Chronic Inflammation
Acute inflammation is an important part of how your body responds to injuries or infections. Chronic inflammation, however, is harmful. Chronic inflammation occurs when the inflammatory response stays active for prolonged periods of time, leading to swelling, warmth, and pain in the affected area that will not go away.
Chronic inflammation is generally caused by one of four things:
- Unhealed injury - Injuries such as a serious tear in a ligament that will not heal on its own can lead the inflammatory response to stay active for far longer than it should.
- Repeated reinjury - Someone who has something in their body that causes repeated reinjury, such as a piece of sharp shrapnel that cannot be removed, will experience continuous irritation and reinjury that leads to chronic inflammation. Abnormal bone structure, such as a bone spur, can also have the same effect as foreign bodies.
- Chronic infection - If your body is not able to quickly eliminate an infection, the infection can become chronic. This results in your inflammatory response remaining active and leads to chronic inflammation.
- Autoimmune disease - Autoimmune diseases are one of the most frustrating causes of chronic inflammation, as they are very difficult to treat.
Chronic inflammation causes a continuous element of stress on the body while also generating near-constant pain. This can make dealing with chronic inflammation a complicated and unpleasant experience.
Inflammatory Diseases
There are many different types of inflammatory diseases that can affect almost every part of your body. Most inflammatory diseases are autoimmune, caused by an overreactive immune system that is attacking a particular type of the person’s own tissues. Many of the common inflammatory diseases affect the joints, but all parts of the body can be impacted by inflammation.
Osteoarthritis

Osteoarthritis [5] is the most common form of arthritis and is caused because cartilage wears down and becomes damaged. Cartilage lines the surface of the ends of each bone, helping the bones to slide smoothly across each other as they move. With osteoarthritis, the cartilage wears down, and the bones scrape against each other as they move.
The symptoms of osteoarthritis include:
- Pain in a specific joint
- Stiffness in the joints
- Swelling
- Crepitus (a creaking, grating sensation in the joints)
- Decreased range of motion
The inflammation associated with osteoarthritis occurs because of the repeated injury that occurs when two bones rub directly against each other without the cushioning effect that cartilage provides.
The cause of osteoarthritis is not fully understood; however, medical researchers do know that it is not caused just by normal wear and tear. Often, repeated movement or injury to the affected joint occurs before osteoarthritis develops.
Treatment for osteoarthritis involves treating pain using non-opioid pain medicines that help reduce inflammation, using physical therapy to optimize the function of the joint, and sometimes surgically replacing the affected joint.
Rheumatoid Arthritis
Rheumatoid arthritis [6] is the second most common form of arthritis, following osteoarthritis. This form of arthritis is an autoimmune condition in which the body’s immune system attacks the lining of your joints. This leads to chronic inflammation in the joint and causes chronic pain.
The symptoms of rheumatoid arthritis include:
- Pain in multiple joints on both sides
- Stiffness in the joints
- Swelling
- Fever
- Fatigue
Unlike osteoarthritis, the symptoms of rheumatoid arthritis will generally occur bilaterally, being the same on both sides of the body. For example, if rheumatoid arthritis is just present in your hands, it will generally affect both hands equally.
The cause of rheumatoid arthritis is due to an autoimmune condition. With this disease, the immune system attacks the normal, healthy tissues that line the affected joints. This leads to chronic inflammation that creates swelling. The swelling leads to pain in the joint and stiffness when moving.
Treatment for rheumatoid arthritis involves treating pain and using medicines that can suppress the immune system. Steroids can be used to suppress the overactive immune system; However, other drugs that are stronger may also be used. The one important consideration is that while suppressing the immune system can help treat rheumatoid arthritis, it can also make you more prone to getting infections.
Gout

Gout [7] is a particularly painful type of arthritis that generally only affects a single joint at a time. Gout is more treatable than rheumatoid arthritis or osteoarthritis but can be debilitating when it occurs.
Symptoms of gout can include:
- Pain that can be very intense
- Swelling of the joint
- Redness over the joint
- Heat in the joint
While gout can affect any joint in your body, it most commonly will affect the great toe.
The cause of gout is the build-up of a chemical called uric acid in your blood. Uric acid begins to crystalize in your joint, creating long, spiky crystals that tear up the tissues around the joint, especially when the joint is moved. This repeated source of injury causes inflammation as long as the crystals remain.
Treatment for gout involves using medicines to reduce levels of uric acid, but more importantly it involves dietary changes. Foods high in purines lead to the production of uric acid, and avoiding these foods can reduce levels of uric acid, helping to avoid future episodes of gout. The pain from gout can be treated using non-opioid anti-inflammatory medicines.
Systemic Lupus Erythematosus

Systemic lupus erythematosus (SLE) [8] is often just referred to as lupus, however, the term lupus actually encompasses other types of lupus besides SLE. SLE is the worst and most common form of lupus and can lead to serious health problems.
Symptoms of systemic lupus erythematosus can include:
- Rashes, especially a butterfly-shaped rash over the cheeks and nose
- Inflammation of the joints
- Swelling in the feet, legs, and around the eyes
- Severe fatigue
- Low-grade fevers
- Heart problems
- Stroke
- Memory problems
- Kidney problems
SLE can affect every area of the body and generally affects connective tissues that are found in almost every organ. SLE symptoms can range from mildly unpleasant to potentially fatal.
The cause of systemic lupus erythematosus is autoimmune-based. In someone with SLE, the immune system becomes overactive, targeting connective tissue. This can affect the skin, the kidneys, the heart, brain tissues, blood vessels, and many other organs. SLE causes inflammation throughout the body and makes the body attack itself. This can cause important organs to become so damaged they do not function correctly and lead to serious injuries in severe cases.
Treatment for systemic lupus erythematosus can be difficult, as there is no cure for the condition. Lifestyle changes, such as sun protection, following a healthy diet, and avoiding illnesses, can help reduce the frequency and severity of flares. Medicines that suppress the immune system, such as steroids and stronger immunosuppressants, can also help treat SLE, however, these medicines can lead to complications and increased risks of infection. Ultimately, SLE treatment focuses on improving the quality of life and avoiding serious complications of the condition.
Chronic Infection
Chronic infection [9] is a broad term that can include bacterial infections that are difficult to treat or viral infections that cannot be irradiated. Diseases like human immunodeficiency virus (HIV) infection or hepatitis C may result in infections that cannot be cured or that will not resolve without treatment. Most chronic infections will lead to chronic inflammation, with HIV being a rare exception because it suppresses the immune system and inflammatory response.
Symptoms of a chronic infection include:
- An injury that doesn’t seem to heal
- An injury with pus
- An injury with a foul smell
- Frequent or persistent fevers
- Fatigue
A more systemic chronic infection, such as shingles or hepatitis, is likely to have symptoms that are very specific to the particular type of infection that is present. Most chronic infections will lead to chronic inflammation unless the infection specifically surpasses the immune system.
The cause of chronic infections is an infection developing that the immune system is not able to take care of. This can be due to a weak immune system that is not able to deal with an infection that it should be able to. However, this can also be due to specific types of infections that are able to evade the immune system.
Treatment for chronic infections depends entirely on the type of infection. Bacterial infections can be treated using antibiotics but may also require surgery or special wound dressings. Some infections will require specific antiviral medications or other medicines that are specific to the type of organism causing the infection.
Psoriasis

Psoriasis [10] is a skin condition in which skin cells build up, creating red, scaly patches. These patches can be uncomfortable, itchy, and cosmetically undesirable. While psoriasis is not generally dangerous, it can be unpleasant to have to deal with.
Symptoms of psoriasis often include:
- Rashes with varying colors
- Dry, cracked skin
- Bleeding from cracked skin
- Itching
- Burning
- Soreness
- Scaly skin
Psoriasis can mimic many other types of skin conditions making it more complicated to distinguish from other similar diseases.
The cause of psoriasis is autoimmune, causing inflammation to skin cells and making them reproduce too quickly. This leads the extra skin cells to build up and causes the alterations in the skin that occur with psoriasis.
Treatment for psoriasis involves using medicines to help reduce the autoimmune response that causes skin cells to reproduce too quickly, using topical ointments to help slow the growth of skin cells, and ultraviolet light treatments that help inhibit skin cell growth.
Chronic Injuries
Chronic injuries [11] are not technically an inflammatory disease but bear consideration as a significant source of inflammation. Chronic injuries typically describes injuries that will not heal correctly on their own and exist for a prolonged period of time.
Chronic injuries can describe a wide number of conditions but will often involve some form of tearing of a ligament or cartilage. These types of injuries will often not heal on their own, especially if they are more than minor injuries. In an attempt to promote healing, the body may create chronic inflammation. These injuries may also increase the likelihood of future injuries affecting the same area. This can lead to prolonged inflammation.
The treatment for chronic injuries varies significantly based on the type of injury. Often, anti-inflammatory medications or heat and cold therapy are used to treat the pain that these injuries cause. Some injuries may require surgical intervention to heal.
Internal Organ Inflammation
There are many organ-specific inflammatory diseases that are too numerous to cover in detail. Many types of organ-specific inflammation are commonly associated with specific causes, such as a specific virus or alcohol use. These conditions can normally be identified because they begin with a root that includes the name of the organ and end with -itis, indicating inflammation.
Some of the most common organ-specific inflammatory diseases include:
- Pancreatitis - Inflammation of the pancreas. Frequently caused by heavy alcohol use.
- Hepatitis - Inflammation of the liver. Typically caused by either a certain type of viral infection or by heavy alcohol use.
- Endocarditis - Inflammation of the inner layer of the heart. Generally caused by bacterial infections, often after a dental infection or dental procedure.
- Asthma - Inflammation of the lining of the airways. It is thought to be primarily an autoimmune condition and occurs in flares rather than as a chronic condition.
- Inflammatory bowel disease - Inflammation of the bowel. The cause is unknown but is thought to be at least somewhat autoimmune-driven.
While these conditions are some of the more common types of organ-related inflammation, there are many other kinds of organ-specific inflammation that someone may experience.
Red Light Therapy and Inflammation
There are many different ways that red light therapy is thought to help inflammation, and research on the topic continues to emerge. Promoting wound healing is the first use of red light therapy that was discovered, and improved inflammatory response may have played a role in that initial discovery.
How Might Red Light Therapy Help Inflammation?
Every molecule absorbs specific wavelengths of light. Plants use this effect to capture sunlight and use photosynthesis to produce energy; retinal cells use this effect to detect light and send signals to the brain to create sight; and skin cells use this effect to absorb ultraviolet light and use the energy to create vitamin D.
Red light therapy is thought to work by creating wavelengths of light absorbed by a chemical called cytochrome C oxidase. [12] This chemical is found in mitochondria - small organs found in almost every cell. Cytochrome C oxidase plays a vital role in helping the mitochondria produce energy, and using the red and infrared wavelengths of light that red light therapy uses is thought to improve mitochondrial function. The mitochondria play a key role in inflammation [13]. Promoting good mitochondrial function could help them to reduce inflammatory signaling and help to reduce inflammation.
In addition to stimulating cytochrome C oxidase, red light therapy is also thought to enhance melatonin production [14] in cells. This melatonin does not enter the bloodstream like the melatonin that promotes sleep but is thought to remain within the cell. Melatonin is a powerful antioxidant, and the effects of stimulating melatonin production may play an important role in how red light therapy could suppress inflammation.
Red Light Therapy and Osteoarthritis

Red light therapy has long been thought to be a helpful treatment for people who suffer from osteoarthritis. This is one of the most established antiinflammatory applications of red light therapy and several studies have found that using red light therapy improves symptoms of osteoarthritis.
One of the oldest studies [16] in this area was published in 1992 in the Journal of the American Geriatrics Society. The study was a partially double-blinded, fully randomized trial comparing red, infrared, and placebo light emitters. It involved 50 patients with age-related knee pain and osteoarthritis and demonstrated that the treatment was “effective in relieving pain and disability in degenerative osteoarthritis of the knee.”
A large study analyzing 22 different studies using red light therapy to treat osteoarthritis found that “the majority of groups that received laser showed significant improvements in pain, function, and quality of life when compared with placebo or control.” This study [17], published in Geriatric Rehabilitation, found that the results varied between studies but supported the use of red light therapy as an effective means of managing osteoarthritis pain.
One study [18] published in Sage Journals using animal models found that red light therapy may not just suppress pain by suppressing inflammation but may actually help restore the health of damaged cartilage in those who have osteoarthritis.
A 2013 study [19], published in BMC, examined the results of using red light therapy to treat osteoarthritis in rats. This research demonstrated that “a single application of [red light therapy] produced significant reductions in inflammatory cell infiltration and inflammatory cytokines 24 hours later.”
Research [20] performed in Saudi Arabia in 2017 and published in Lasers in Medical Science shows that red light therapy could improve osteoarthritic pain by creating chemical changes. Their results als showed improving cartilage thickness following treatment.
Another study [21], published in Clinical Rheumatology, studied the use of red light therapy to treat cervical osteoarthritis, a particularly unpleasant form of osteoarthritis affecting the neck. This study was controlled and followed 60 patients, ultimately indicating that red light therapy could be used to relieve pain and improve function with this painful condition.
A metastudy [22] published in Alternative Therapies in Health and Medicine examined dozens of studies that tested the use of red light therapy for osteoarthritis, covering research from 1996 to 2016. This literature review concluded, “Based on current research, the utilization of [red light therapy] for pain management and osteoarthritic conditions may be a complementary strategy used in clinical practice to provide symptom management for patients suffering from osteoarthritis and chronic pain.”
Red Light Therapy and Rheumatoid Arthritis
Multiple studies have found that red light therapy can help improve symptoms in people who have rheumatoid arthritis. A study [23] published in Laser Therapy found that using infrared light reduced expressions of IL-20, a gene known to be involved in causing rheumatoid arthritis.
Another study [24] in the journal Nanoscale showed that using red light therapy to treat rheumatoid arthritis may help inhibit or even destroy inflammatory cells that promote the inflammation caused by rheumatoid arthritis.
Research [25] published in The Journal of Rheumatology found that using four to ten weeks of red light therapy could help improve both pain and disease activity in people who suffered from rheumatoid arthritis. Symptoms like morning stiffness, flexibility, and swelling were all found to be improved after using red light therapy.
A 2009 study [26] in Lasers in Surgery and Medicine found that red light therapy can improve pain caused by rheumatoid arthritis. The researchers found that red light therapy improved certain biomarkers and proposed that the mechanism for joint pain relief may involve red light therapy reducing the level of pro-inflammatory cytokines/chemokines produced by cells that line the joint.
A 2013 publication in Arthritis Research & Therapy provided an animal model study [27] demonstrating that the way that red light therapy improved joint pain could involve modulation of inflammatory mediators and inflammatory cells. By reducing the activity of cells and chemicals that cause inflammation, pain and effects of inflammation could be reduced.
A meta analysis [28] of research into the use of red light therapy to treat joint pain was published in the Journal of Physiotherapy. This study found that red light therapy was helpful in reducing joint pain and improving health status in chronic joint disorders; however, it also cautious interpretation of the results of existing studies and suggested that further research would be necessary.
Red Light Therapy and Musculoskeletal Injuries

Red light therapy has shown extensive promise in the area of improving joint and muscle health. While it is used as a workout recovery tool, it also shows promise in helping to treat sprains and strains. A study [29] in the Journal of Sport Rehabilitation showed that red light therapy was superior in promoting workout recovery when compared to cryotherapy, demonstrating an improved inflammatory response. Another study in PLOS One demonstrated that using red light therapy provided an anti-oxidative effect on muscles, helping them to heal more quickly after sports injuries.
Research [30] published in BMC Sports Science, Medicine and Rehabilitation also found that there is evidence that red light therapy can be used to help treat tendinopathy disorders. This study was a meta-analysis - a large study that analyzes multiple studies for patterns.
A master’s thesis [31] performed in 2007 by Elisabeth A. Martin of Cedarville University examined the effectiveness of using red light therapy to treat inflammation caused by lower extremity sprains and strains of college athletes. The research found that “light therapy is an effective modality for use with acute pain of acute lower extremity sprains and strains.”
Red Light Therapy and Skin Inflammation
Red light therapy has been shown to help with different types of skin inflammation and diseases that cause skin inflammation. Red light therapy has been shown to help treat psoriasis and the redness of the skin that it creates. A study [32] published in the Journal of the European Academy of Dermatology and Venereology compared the effects of red light and blue light when treating psoriasis, finding that their effects were similar but that blue light therapy had a longer duration of action. These results support the idea of combining the benefits of red light therapy with already-established blue light therapy when treating the inflammation caused by psoriasis.
Another research initiative [33] published in the Journal of the European Academy of Dermatology and Venereology found that red light therapy helped to reduce symptoms of rosacea. Rosacea is a skin condition that is driven by inflammation, and the anti-inflammatory effects of red light therapy likely play an important role in how it helps those with rosacea.
A 2016 study [34] in Photodermatology, Photoimmunology, & Photomedicine examined how red light therapy promoted wound healing. The researchers ultimately determined that reduced inflammation was one of the key ways that red light therapy facilitates wound healing.
Other Anti-Inflammatory Effects of Red Light Therapy
While there are several commonly used anti-inflammatory applications for red light therapy, there have been numerous studies into other areas as well. These include inflammation in the brain, the ear, the intestines, and even a type of inflammation caused by some COVID-19 infections. Most of these new areas of study are quite recent compared to well-established uses of red light therapy for inflammation.
Some of the more prominent studies for other antiinflammatory applications of red light therapy include:
- In 2020, a study [35] was published in the Journal of Photochemistry and Photobiology B: Biology examining red light therapy for colitis in mice. Colitis is a chronic inflammatory disease affecting the colon. The study found that red light therapy inhibited mediators of inflammation and showed potential as a possible method for treating colitis.
- In 2021, a study [36] published in Communicative & Integrative Biology demonstrated that the use of red light therapy effectively suppressed TLR-4 dependent inflammation, a type of inflammation commonly associated with severe COVID-19 infections. While the study didn’t directly study red light therapy in COVID-19 patients, it may potentially lead to red light therapy-based COVID-19 treatment options in the future.
- In 2022, a study [37] published in Scientific Reports examined the effects of red light therapy on brain inflammation that was deliberately induced in lab mice. The research showed that red light therapy resulted in the modulation of neuroinflammation by suppressing glia cell activation and reducing pro-inflammatory cytokines, chemicals that can cause inflammation in the brain.
- Another study [39] in 2022, published in Frontiers in Neuroscience, reviewed many other studies on the effects of red light therapy on neuroinflammation. This large-scale study found that red light therapy has anti-inflammatory properties in several conditions. The researchers suggested red light therapy could help treat traumatic brain injury, edema formation and hyperalgesia, ischemia, neurodegenerative conditions, aging, epilepsy, depression, and spinal cord injury.
A 2023 study [39], published in Frontiers in Bioengineering and Biotechnology, showed that red light therapy improved inflammation in rats for otitis media. Otitis media is a form of ear infection. While the research was in animals, it does suggest the potential that this effect could occur in humans and should be tested further.
How is Red Light Therapy Used?
Using red light therapy to improve inflammation is so easy that almost anyone can do it. Prior to using red light therapy, there are a few steps that you should take:
- Consider possible contraindications - While red light therapy is considered to be quite safe, there are some unique situations in which it is not best to use. Ensure that you do not have any contraindications to red light therapy before using it.
- Learn about red light therapy - There are many important nuances to red light therapy and different considerations based on how you are using it. Taking some time to research red light therapy will help optimize your treatments.
- Ensure consistent access to red light therapy. Red light therapy takes a few weeks of treatment to be effective. Having consistent access to red light therapy is important to be able to see meaningful results.
When you are ready to start using red light therapy, actually treating yourself is quite simple.
- Turn the red light source on.
- Ensure you have protective eyewear on.
- Ensure the area being treated is free of clothing and creams or makeup.
- Position yourself about 6-18 inches from the source.
- Use the treatment for 5-20 minutes.
- Repeat treatments regularly, from three to seven times a week.
Different red light manufacturers may have slight differences in specific distances from the source and timing for treatments. You should always follow the advice of the manufacturer or your physician when using red light therapy.
Mito Red Light
While Mito Red Light therapy devices have not been clinically studied or validated to reduce inflammation, our high quality red light therapy lights deliver the wavelength bands of light that have been shown in studies to potentially help inflammation.
Red light therapy supports cellular energy production. In conjunction with a healthy lifestyle, red light therapy can have a positive impact on your body’s natural response to inflammation.
Our panels are designed to provide the maximum amount of the right wavelengths of light to as much area as possible.
We welcome you to review our selection of high-quality products or to contact one of our expert representatives at +1 866-861-6486.
Related Articles:
- What Is Red and Near Infrared (NIR) Light Therapy?
- Red Light Therapy Buyer’s Guide
- Everything You Need to Know About Red Light Therapy and SKIN
- Top Tips for Optimal Joint Health
References:
- Cotler, H. B. (2015). A NASA discovery has current applications in orthopaedics. Current Orthopaedic Practice, 26(1), 72-74. https://doi.org/10.1097/BCO.0000000000000196
- Tafur, J., & Mills, P. J. (2008). Low-Intensity Light Therapy: Exploring the Role of Redox Mechanisms. Photomedicine and Laser Surgery, 26(4), 323-328. https://doi.org/10.1089/pho.2007.2184
- MedlinePlus. (n.d.). Immune response. U.S. National Library of Medicine. Retrieved June 29, 2023, from https://medlineplus.gov/ency/article/000821.htm
- National Institute of Environmental Health Sciences. (n.d.). Inflammation. Retrieved June 29, 2023, from https://www.niehs.nih.gov/health/topics/conditions/inflammation/index.cfm
- Centers for Disease Control and Prevention (n.d.). Osteoarthritis (OA). Retrieved June 29, 2023, from https://www.cdc.gov/arthritis/
- Centers for Disease Control and Prevention. (2020). Rheumatoid arthritis (RA). Retrieved June 29, 2023, from https://www.cdc.gov/arthritis/
- Centers for Disease Control and Prevention. (2020). Gout. Retrieved June 29, 2023, from https://www.cdc.gov/arthritis/
- Lupus Foundation of America. (n.d.). What is systemic lupus erythematosus (SLE)? Retrieved June 29, 2023, from https://www.lupus.org/resources/what-is-systemic-lupus-erythematosus-sle
- Reese, T.A.. (n.d.). Chronic Viral Infections vs. Our Immune System: Revisiting our view of viruses as pathogens. Retrieved June 29, 2023, from https://www.utsouthwestern.edu/education/programs/stars/assets/Dr.%20Tiffany%20Reese.pdf
- Centers for Disease Control and Prevention. (2020). Psoriasis. Retrieved June 29, 2023, from https://www.cdc.gov/psoriasis/
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (n.d.). Niams health information on sports injuries. Retrieved June 29, 2023, from https://www.niams.nih.gov/health-topics/sports-injuries
- Mason, M. G., Nicholls, P., & Cooper, C. E. (2014). Re-evaluation of the near infrared spectra of mitochondrial cytochrome c oxidase: Implications for non invasive in vivo monitoring of tissues. Biochimica et Biophysica Acta (BBA) - Bioenergetics, 1837(11), 1882–1891. https://doi.org/10.1016/j.bbabio.2014.08.005
- Missiroli, S., Genovese, I., Perrone, M., Vezzani, B., Vitto, V. A. M., & Giorgi, C. (2020). The Role of Mitochondria in Inflammation: From Cancer to Neurodegenerative Disorders. Journal of Clinical Medicine, 9(3), 740. https://doi.org/10.3390/jcm9030740
- Hamblin, M. R. (2017). Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophysics, 4(3), 337–361. https://doi.org/10.3934/biophy.2017.3.337
- Yeager, R. L., Oleske, D. A., Sanders, R. A., Watkins 3rd, J. B., Eells, J. T., & Henshel, D. S. (2007). Melatonin as a principal component of red light therapy. Medical Hypotheses, 69(2), 372-376. https://doi.org/10.1016/j.mehy.2006.12.041
- Stelian, J., Gil, I., Habot, B., Rosenthal, M., Abramovici, I., Kutok, N., & Khahil, A. (1992). Improvement of pain and disability in elderly patients with degenerative osteoarthritis of the knee treated with narrow-band light therapy. Journal of the American Geriatrics Society, 40(1), 23-26. https://doi.org/10.1111/j.1532-5415.1992.tb01824.x
- Bridges, M., Hilliard, J., & Chui, K. (2020). Effects of Light Therapy on Osteoarthritis and Its Sequelae in Aging and Older Adults: A Systematic Narrative Review. Topics in Geriatric Rehabilitation, 36(1), 11-37. https://doi.org/10.1097/TGR.0000000000000251
- Balbinot, G., Schuch, C. P., ... & Vaz, M. A. (2019). Photobiomodulation Therapy Partially Restores Cartilage Integrity and Reduces Chronic Pain Behavior in a Rat Model of Osteoarthritis: Involvement of Spinal Glial Modulation. Cartilage, 13(2_suppl). https://doi.org/10.1177/1947603519876338
- Hamblin, M. R. (2013). Can osteoarthritis be treated with light? Arthritis Research & Therapy, 15, 120. https://doi.org/10.1186/ar4354
- Nambi, G. S., Kamal, W., George, J., & Manssor, E. (2017). Radiological and biochemical effects (CTX-II, MMP-3, 8, and 13) of low-level laser therapy (LLLT) in chronic osteoarthritis in Al-Kharj, Saudi Arabia. Lasers in Medical Science, 32(2), 297-303. https://doi.org/10.1007/s10103-016-2114-5
- Ozdemir, F., Birtane, M., & Kokino, S. (2001). The clinical efficacy of low-power laser therapy on pain and function in cervical osteoarthritis. Clinical Rheumatology, 20(3), 181-4. https://doi.org/10.1007/s100670170061
- Dima, R., Francio, V. T., Towery, C., & Davani, S. (2018). Review of literature on low-level laser therapy benefits for nonpharmacological pain control in chronic pain and osteoarthritis. Alternative Therapies in Health and Medicine, 24(5), 8-10. Retrieved June 29, 2023, from https://pubmed.ncbi.nlm.nih.gov/28987080/
- Imaoka, A., Zhang, L., Kuboyama, N., & Abikocorresponding, Y. (2014). Reduction of IL-20 expression in rheumatoid arthritis by linear polarized infrared light irradiation. Laser Therapy, 23(2), 109–114. https://doi.org/10.5978/islsm.14-OR-08
- Dong, Y., Cao, W., & Cao, J. (2021). Treatment of rheumatoid arthritis by phototherapy: advances and perspectives. Nanoscale, (35). Retrieved June 29, 2023, from https://pubs.rsc.org/en/content/articlelanding/2021/nr/d1nr03623h#!divCitation
- Brosseau, L., Welch, V., Wells, G., Tugwell, P., de Bie, R. A., Gam, A., Harman, K., Shea, B. J., & Morin, M. (2000). Low level laser therapy for osteoarthritis and rheumatoid arthritis: A metaanalysis. The Journal of Rheumatology, 27(8), 1961-9. Retrieved June 29, 2023, from https://pubmed.ncbi.nlm.nih.gov/10955339/
- Yamaura, M., Yao, M., Yaroslavsky, I., Cohen, R., Smotrich, M., & Kochevar, I. E. (2009). Low level light effects on inflammatory cytokine production by rheumatoid arthritis synoviocytes. Lasers in Surgery and Medicine, 41(4), 282-90. https://doi.org/10.1002/lsm.20766
- Alves, A. C., Vieira, R., Leal-Junior, E., dos Santos, S., Ligeiro, A. P., Albertini, R., Junior, J., & de Carvalho, P. (2013). Effect of low-level laser therapy on the expression of inflammatory mediators and on neutrophils and macrophages in acute joint inflammation. Arthritis Research & Therapy, 15(5), R116. https://doi.org/10.1186/ar4296
- Bjordal, J. M., Couppé, C., Chow, R. T., Tunér, J., & Ljunggren, E. A. (2003). A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Australian Journal of Physiotherapy, 49(2), 107-16. https://doi.org/10.1016/s0004-9514(14)60127-6
- Fisher, S. R., Rigby, J. H., Mettler, J. A., & McCurdy, K. W. (2019). The Effectiveness of Photobiomodulation Therapy Versus Cryotherapy for Skeletal Muscle Recovery: A Critically Appraised Topic. Journal of Sport Rehabilitation, 28(5), 526–531. https://doi.org/10.1123/jsr.2017-0359
- Tripodi, N., Feehan, J., Husaric, M., Sidiroglou, F., & Apostolopoulos, V. (2021). The effect of low-level red and near-infrared photobiomodulation on pain and function in tendinopathy: a systematic review and meta-analysis of randomized control trials. BMC Sports Science, Medicine and Rehabilitation, 13, Article number: 91. https://doi.org/10.1186/s13102-021-00306-z
- Martin, E. A. (2007). Light Therapy: The Effectiveness of Light Therapy on Pain and Swelling of Acute Lower Extremity Sprains and Strains of Collegiate Athletes. Cedarville University, Master of Education Research Theses Master of Education Capstones. Retrieved June 29, 2023, from https://digitalcommons.cedarville.edu/cgi/viewcontent.cgi?article=1013&context=education_theses
- Kleinpenning, M. M., Otero, M. E., van Erp, P. E. J., Gerritsen, M. J. P., & van de Kerkhof, P. C. M. (2012). Efficacy of blue light vs. red light in the treatment of psoriasis: a double-blind, randomized comparative study. Journal of the European Academy of Dermatology and Venereology, 26(2), 219-25. https://doi.org/10.1111/j.1468-3083.2011.04039.x
- Bryld, L. E., & Jemec, G. B. E. (2007). Photodynamic therapy in a series of rosacea patients. Journal of the European Academy of Dermatology and Venereology, 21(9), 1199-1202. https://doi.org/10.1111/j.1468-3083.2007.02219.x
- Yadav, A., & Gupta, A. (2017). Noninvasive red and near-infrared wavelength-induced photobiomodulation: promoting impaired cutaneous wound healing. Photodermatology, Photoimmunology, & Photomedicine, 33(1), 4-13. https://doi.org/10.1111/phpp.12282
- de Paula-Silva, M., Broering, M. F., Scharf, P., da Rocha, G. H. O., Farsky, S., & Lino-dos-Santos-Franco, A. (2020). Red light-emitting diode treatment improves tissue recovery in DSS-induced colitis in mice. Journal of Photochemistry and Photobiology B: Biology, 212, 112018. https://doi.org/10.1016/j.jphotobiol.2020.112018
- Aguida, B., Pooam, M., Ahmad, M., & Jourdan, N. (2021). Infrared light therapy relieves TLR-4 dependent hyper-inflammation of the type induced by COVID-19. Communicative & Integrative Biology, 14(1), 200-211. https://doi.org/10.1080/19420889.2021.1965718
- Saieva, S., & Taglialatela, G. (2022). Near-infrared light reduces glia activation and modulates neuroinflammation in the brains of diet-induced obese mice. Scientific Reports, 12, 10848. https://doi.org/10.1038/s41598-022-14812-8
- Cardoso, F. dos S., Salehpour, F., Coimbra, N. C., Gonzalez-Lima, F., & da Silva, S. G. (2022). Photobiomodulation for the treatment of neuroinflammation: A systematic review of controlled laboratory animal studies. Frontiers in Neuroscience, 16. https://doi.org/10.3389/fnins.2022.1006031
39. Ko, Y.-S., Gi, E.-J., Lee, S., & Cho, H.-H. (2023). Dual red and near-infrared light-emitting diode irradiation ameliorates LPS-induced otitis media in a rat model. Frontiers in Bioengineering and Biotechnology, 11. https://doi.org/10.3389/fbioe.2023.1099574